Recognizing and Treating the Psychological Effects of Stroke
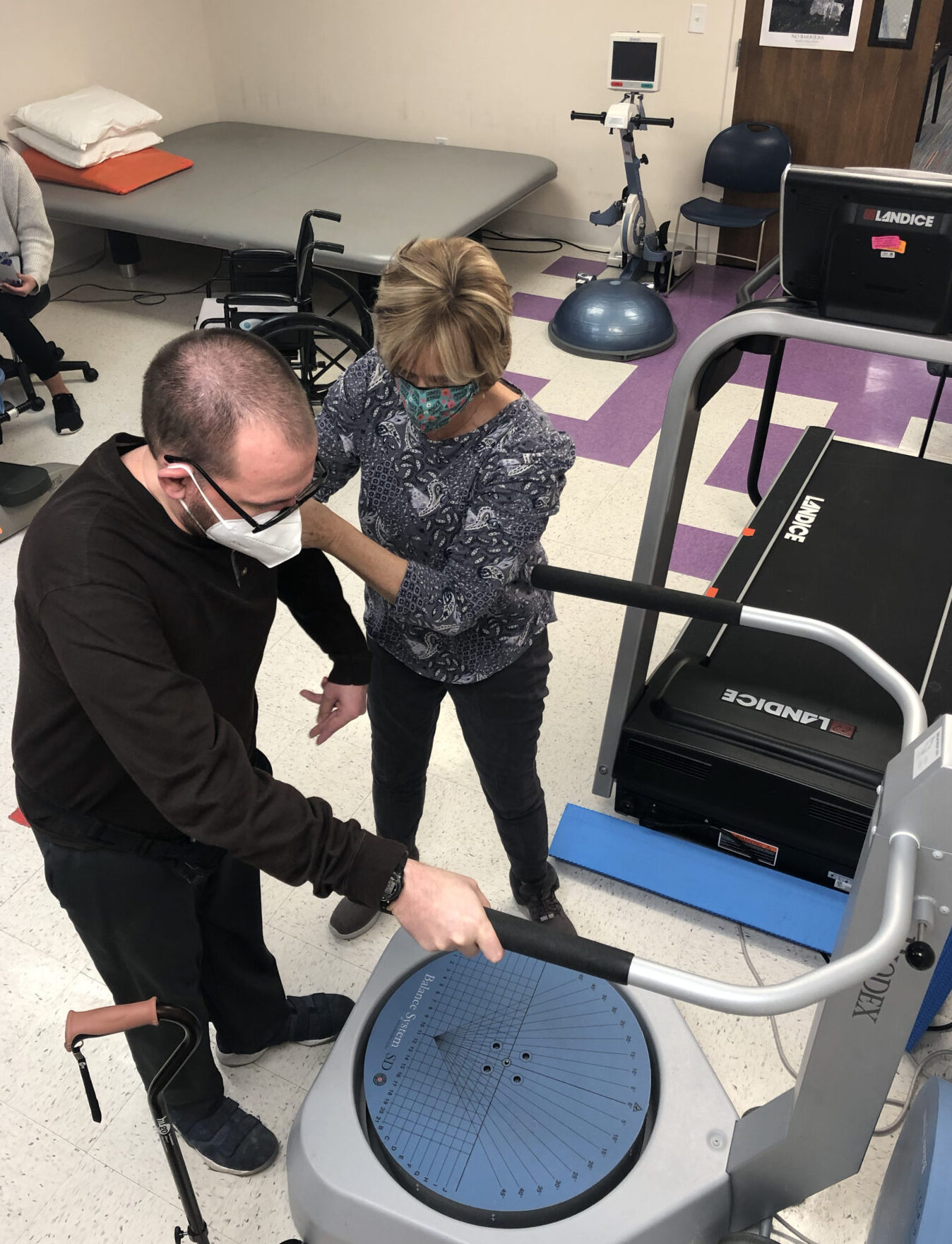
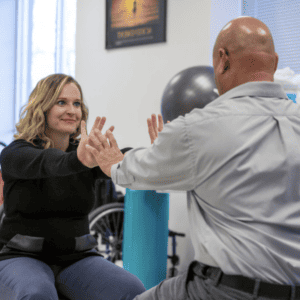
Post-Stroke Rehabilitation
Stroke recovery may conjure images of a patient working hard to overcome physical- or speech-related difficulties or deficits caused by the event. While physical, occupational and speech therapy are important aspects of a patient’s rehabilitation, it is important to consider the potential psychological and emotional impacts patients may encounter on their road to recovery.
The myriad psychological and emotional challenges patients face during their recovery may reflect some of the neurological changes caused by the stroke itself or may develop as a patient faces and copes with the changes in their life and abilities related to their injury.
Strokes may cause an array of neuropsychiatric symptoms depending on the specific type of syndrome a patient experiences, although middle cerebral artery (MCA) strokes account for about two-thirds of all stroke events. The mood and behavior changes stemming from MCA, anterior cerebral artery and other forms of stroke can affect the frontal lobes of the brain and the connections with the limbic system that, in turn, may cause a patient to experience emotional and behavioral changes.
Understanding the Neuropsychiatric Symptoms Caused by a Stroke
Understanding and recognizing the symptoms caused by a stroke is crucial for brain recovery, such as sudden numbness or weakness, especially on one side of the body, can aid in early intervention. Being aware of the cognitive deficits in post-stroke, like memory loss or difficulty with problem-solving, can help in providing appropriate support. Additionally, understanding the impact of stroke on daily activities, such as bathing, dressing, and cooking, is essential for facilitating recovery and improving the quality of life for stroke survivors.
The most common neuropsychiatric symptoms following a stroke include:
- Confusion
- Irritability
- Denial of deficits
- Hallucinations
- Delusions
- Restlessness/agitation
- Indifference or euphoria
- Difficulty understanding tones and emphasis in speech
- Depression
- Lack of motivation
- Hyperactivity
- Excessive talking/verbosity
- False memories
- Impaired judgement
Can a Stroke Cause Depression?
The most commonly observed psychological or behavioral syndrome following a stroke is called post-stroke depression (PSD). A significant portion of stroke survivors may face the challenges of depression for an extended period, impacting their overall well-being and quality of life. Therefore, it becomes crucial to address and effectively manage post-stroke depression as part of the rehabilitation and recovery process.
By recognizing the persistent nature of depression in stroke survivors, healthcare professionals can provide the necessary support and interventions to improve emotional changes after a stroke.
The post-stroke depression symptoms mirror those of major depression and may include:
- Low mood
- Decreased interest in activities
- Weight changes
- Appetite changes
- Sleep problems
- Restlessness
- Fatigue
- Feelings of worthlessness
- Feelings of guilt
- Concentration and memory problems
- Thoughts of death


The Impact of Stroke Recovery and the Effects of Post-Stroke Depression
It’s crucial to acknowledge the wide variation in the occurrence of post-stroke depression and its relationship with the duration of stroke recovery. Studies vary on the prevalence of post-stroke depression into the chronic phase – a year or more after the event. Some studies place the prevalence at around 18% of patients while other studies estimate more than 50% of patients suffer from longer-term depression.
Research demonstrates that depression is associated with a higher mortality rate among stroke survivors. Although their rate of suicide is less than those diagnosed with major depression, the risk is still higher for post-stroke depression patients than for the general population.
When any symptoms of depression arise, healthcare providers should evaluate whether the symptoms are directly related to the stroke, to depression itself, or a combination of both. The complexities and impact of a stroke and the adjustments made by patients as they recover highlight the need for providers who fully understand neurologic injuries as well as the potential psychological effects of a stroke.


Post-Stroke Depression Risk Factors
While it is not possible to predict who may develop depression after a stroke, several factors increase the risk of developing the condition, including:
- Stroke severity
- Poor functional status
- Impaired daily living skills
- Low education and income status
- Pre-stroke history of depression/psychiatric illness
- Family history of psychiatric illness
- Pre-stroke cerebral atrophy
Post-stroke depression can hinder a person’s recovery if it limits their ability and motivation to engage in activities that support their rehabilitation. Those who are less physiologically engaged and less physically active may also be considered potential risk factors for predictors of worse outcomes following stroke.
Treatment Approaches for Post-Stroke Depression
There are many approaches available to help those who have suffered a stroke and are experiencing depression or have other behavioral syndromes caused by the event.
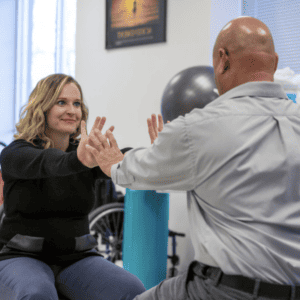
Psychotherapy
Psychotherapy offers patients a pathway to help them cope with any personal problems or difficulties they are experiencing and helps them explore ways to manage their depression symptoms. It is important that patients receive treatment from a therapist or a psychologist with specialized training in neuropsychology, the various stroke syndromes and how they affect mood and behavior.
Psychotherapy may also help individuals understand their thoughts and feelings so that they can adjust to changes in their functioning and develop a new way to think about and experience the changes they are experiencing. Working closely with a qualified therapist can also help foster a positive sense of one’s capacities and abilities and explore helpful resources.


Medication Options
Common antidepressants like nortriptyline, trazodone and a class of medicines called serotonin reuptake inhibitors, or SSRIs, can help improve the mood and manage other psychiatric symptoms of those who have post-stroke depression.
Combining medication and psychotherapy with continued physical, occupational and speech therapy helps to reinforce and advance recovery and has the potential to boost an individual’s mood by enhancing their level of activity, engagement and social interaction.
Fortunately, post-stroke depression responds well for many people in response to medications and psychotherapy so getting treatment as soon as possible for depression following a stroke is critical to their recovery and quality of life.
Contact Bancroft NeuroRehab at 844-234-8387 to learn more about our psychotherapy services or to make an appointment.
Related Articles
Navigating Life Beyond Stroke: Shawn’s Story
Navigating Life Beyond Stroke: Shawn’s Story From Mechanic to Patient:


Embracing Balance: How Yoga Supports Brain Injury Recovery
Embracing Balance: How Yoga Supports Brain Injury Recovery The Healing


Never Giving Up: How Stephen Reclaimed His Independence After a Traumatic Brain Injury
Never Giving Up: How Stephen Reclaimed His Independence After a