Stroke
Home » Conditions Treated » Stroke
Overview
A stroke is when blood flow is stopped or reduced to part of the brain. This medical emergency deprives brain cells of oxygen, causing them to start dying within minutes. Immediate treatment is needed to minimize brain damage and other complications.
When brain cells die during a stroke, the person loses abilities controlled by the affected area of the brain – anything from memory to speech, vision to movement. Some people recover fully from a stroke, but more than two-thirds of survivors have long-term effects.
Stroke is the leading cause of disability in the United States, striking 800,000 people a year. But there is good news: More people survive stroke today, and advanced therapies can minimize stroke’s effects.
Contact Us
To make a referral or schedule an appointment call 844-234-8387
Watch as Bancroft NeuroRehab patient, Drew and his wife reflect on getting back their life after a stroke:
Symptoms
Stroke symptoms include:
- Trouble speaking and understanding.
- Paralysis, numbness or weakness of the face, arm or leg. This often happens on just one side of the body.
- Difficulty seeing with one or both eyes, such as blurred, blackened or double vision.
- Sudden, severe headache, which may be accompanied by vomiting, dizziness or reduced consciousness.
- Trouble walking, including stumbling, sudden dizziness, loss of balance or loss of coordination.
When to See a Doctor
If you notice any signs of a stroke, seek emergency medical care immediately – even if the symptoms fluctuate or disappear. Note the time when symptoms began, as the length of time can affect the person’s treatment options.
Take these steps “FAST”:
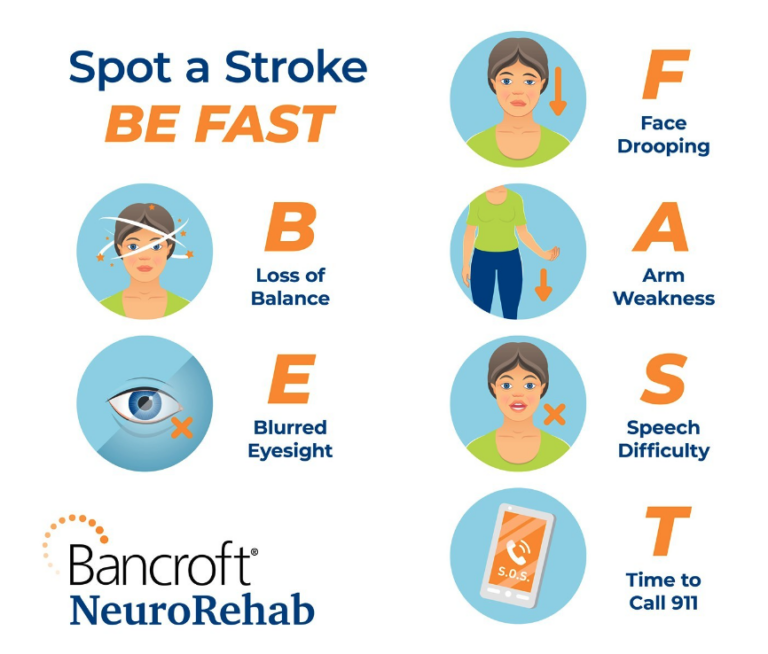
- Face: Ask the person to smile. Does one side of their face droop?
- Arms: Ask the person to raise both arms over their head. Is one arm unable to rise, or does it drift down?
- Speech: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- Time: If you observe any of these signs, call 911 or your local emergency number immediately.
Don’t wait to see if symptoms stop, as every minute counts. The longer a stroke goes untreated, the greater the chance of brain damage and disability. While waiting for emergency help, watch the person carefully.
Causes
Ischemic stroke is often caused by fatty deposits that accumulate inside blood vessels over time – a condition called atherosclerosis. Another common stroke cause is an irregular heartbeat – known as atrial fibrillation – which can lead clots to form in the heart. The clots can break free and travel to the brain.
Hemorrhagic stroke can be caused by high blood pressure, trauma, overuse of blood thinners, weak areas in blood-vessel walls (aneurysms), or rupture of an abnormal blood-vessel formation.
Types of Stroke
The two main kinds of stroke are ischemic stroke and hemorrhagic stroke.
Ischemic stroke, the most common type, occurs when arteries to your brain become narrowed or blocked. For instance, a blood clot can form in an artery that supplies blood to your brain (a thrombotic stroke), or a clot or other deposit can form somewhere else – such as your heart – and then travel to the brain (an embolic stroke).
Hemorrhagic stroke is caused by the leaking or bursting of a blood vessel. For example, an intracerebral hemorrhage is when a blood vessel in the brain ruptures and blood spills into the surrounding brain tissue, damaging brain cells. A subarachnoid hemorrhage is when an artery near the brain’s surface bursts and blood spills into the space between the brain and skull.
A related condition, transient ischemic attack (TIA), can signal an impending stroke. Known as a “mini-stroke,” TIA is a temporary disruption of blood flow to the brain when a clot or debris briefly restricts blood flow. Symptoms may subside in as little as five minutes, and the attack usually does not cause lasting damage. Nevertheless, people should get emergency care for a TIA, as the symptoms are the same as with a true stroke. In addition, 40% of people who have a TIA will have an actual stroke – often within several days of the TIA.
Complications
A stroke can cause a variety of temporary or permanent disabilities, depending on the part of the brain affected and how long the blood flow was interrupted. Complications can include:
- Cognitive issues, such as problems with memory, thinking, understanding, judgment and reasoning.
- Paralysis or loss of movement, including inability to move one side of the body or to control certain muscles. Patients may have trouble walking, talking, eating, swallowing, or performing physical tasks.
- Vision problems, including blurriness, vision loss, and reduced coordination of the two eyes.
- Emotional and behavioral problems, including depression, anxiety, and difficulty controlling one’s emotions. People may withdraw from others or become more impulsive.
- Pain or numbness and other unusual sensations may occur in body parts affected by the stroke. For instance, if your right arm is numb from the stroke, you may also develop tingling in that arm. Survivors may also experience pain from temperature changes, especially severe cold.
- Difficulty with self-care, including trouble with grooming and daily chores due to mental and physical challenges.
Risk Factors
Many factors can increase your risk of having a stroke. On the plus side, some risk factors can be reduced or eliminated through lifestyle changes and/or medical treatment.
Lifestyle factors include inactivity, heavy or binge drinking, smoking or being exposed to secondhand smoke, and using street drugs like cocaine or methamphetamine.
Medical factors include being overweight or obese, high blood pressure, high cholesterol, diabetes, sleep apnea, heart disease, and a personal or family history of stroke, heart attack, or transient ischemic attack.
Other risk factors include being 55 or older, African American, or male, or having higher estrogen levels from birth control pills, estrogen therapies, pregnancy or childbirth.


Life after stroke: A former Flyer shares his story
Brian Propp knows firsthand how devastating a stroke can be – and the difference quality, individualized rehabilitation makes in recovery. Today, Propp hopes to inspire others who are struggling after their own stroke or brain injury as Bancroft NeuroRehab’s brand ambassador.
Treatments and Therapies
A stroke requires immediate treatment to save the person’s life and minimize brain damage. Many stroke survivors also need ongoing therapies to help them regain abilities and live as independently as possible.


Immediate Treatment
Treatment depends on the type of stroke:
With an ischemic stroke – when a clot blocks blood flow to part of the brain – treatment is designed to bust or remove the clot. This can be done with IV (intravenous) medication in the arm, or by physically removing the clot. The medication (Alteplase IV r-tPA) must be given within three hours of the stroke’s onset in most cases. Physical removal of the clot – via a catheter in the body – should be done within six hours of the stroke’s start, and may help up to 24 hours later.
In cases of hemorrhagic stroke – when a blood vessel ruptures within the brain – treatment aims to stop the bleeding. Depending on the situation, this can be done via catheter or conventional surgery.
Post-Stroke Rehabilitation
Rehabilitation is a vital aspect of treatment for most stroke survivors. A range of therapies can help people address the different effects of stroke, including the specific physical, mental, social and emotional challenges they may face. This may include relearning skills, adapting to changes in abilities, or redefining one’s life. The goal: to help people return to their daily activities and independent living.
The first step in post-stroke rehabilitation is a thorough assessment of the survivor’s abilities and deficits, which can include:
Neuropsychological evaluation, a comprehensive, non-invasive test of the person’s mental abilities and mood, including attention and concentration, learning and memory, planning and abstract thinking, language and communication, motor and sensory functions, academic skills, and other intellectual abilities. The test is done through a questionnaire and typically take four to six hours.
PT/OT/SLP/Cognitive evaluations to determine the person’s needs for physical therapy, occupational therapy, and/or speech and language therapy.
Independent medical examination to determine the extent of the stroke and the survivor’s treatment needs.
Once the evaluations are completed, the survivor may receive the following therapies as needed:
Residential rehabilitation, which provides supervised living in the community, with staffing based on the person’s needs. Services can include behavioral programming, social supports, nutritional care, and support and training in daily living skills such as personal care, household management, health and medical care, grocery shopping, money management and budgeting.
Therapeutic day programs, including Individual and group programs that engage in a variety of daily living, vocational, social and recreational activities, designed to help people regain abilities and improve their quality of life. Programs can address communication, thinking skills, back-to-work transition, behavioral issues, community participation, and need for supports or accommodations.
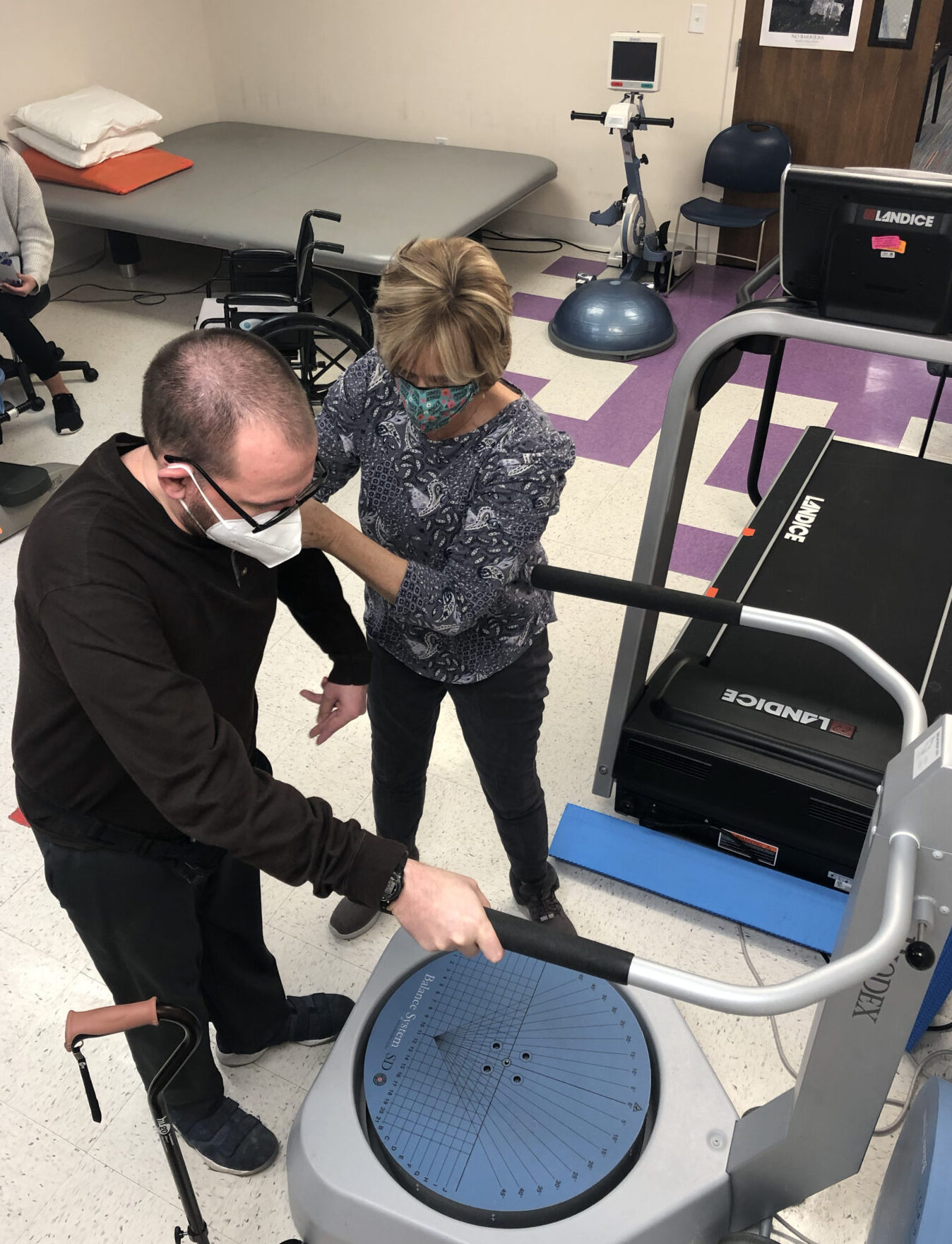
Physical therapy, which restores mobility and improves muscle tone, balance, strength and endurance. Treatment includes enhancing the patient’s walking abilities and/or use of a wheelchair.
Occupational therapy, which restores skills needed to function successfully at home, work or school. Treatment focuses especially on enhancing abilities of the arms, hands and fingers, so survivors can feed, dress and bathe themselves, among other daily tasks.
Speech and language therapy, which improves communication skills and/or swallowing, while also strengthening thinking and memory.
Psychotherapy, which aids in adjustment to the stroke, awareness of deficits, redevelopment of social skills, maintaining of relationships, and education regarding the stroke.
Vestibular therapy, which improves balance and reduces dizziness through exercise.
Vocational rehabilitation, including restoration of job skills and assessment for return to work. Therapists works with both survivor and employer to support the survivor’s re-employment, including onsite job training and job coaching.
Nursing services, which address any medical conditions caused by the stroke and/or pre-existing health issues. Nurses provide medical management of these conditions, oversee medications, and work closely with the survivor’s primary-care provider, neurologist, cardiologist or other specialists.
Neurology, which addresses any new or ongoing symptoms related to the brain or nervous system.
Physiatry, a form of physical medicine that helps patients overcome pain, weakness or disability, and enhances their independence and functioning.
Support groups for survivors and family members, which provide emotional support, practical ideas, motivation and inspiration that can help people thrive after a stroke.
Contact Us
To learn how Bancroft NeuroRehab can help you or a loved one reclaim your life after a stroke, please call 844-234-8387 or click Get Started below.