Concussion: What Every Parent Should Know
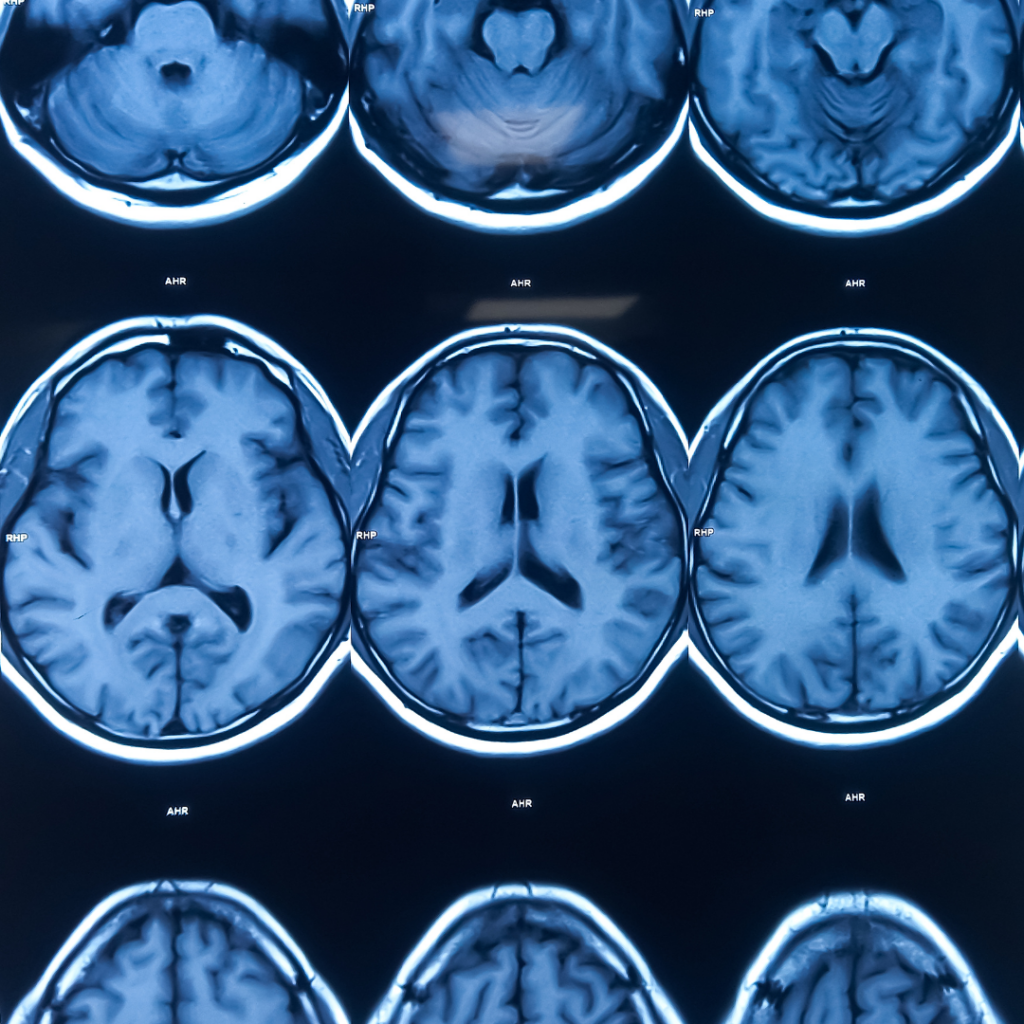
The Beautiful Mind
Brought to you by experts in neurological health, including autism, intellectual and developmental disabilities, and neurological rehabilitation, at Bancroft and Bancroft NeuroRehab: Dr. Claire McGrath and Dr. Sarah West.
Athlete or not; concussions can happen. Two Bancroft NeuroRehab neuropsychologists discuss why the right treatment and rehabilitation is crucial to rebounding, recovering and returning to school and play as soon as possible.
It’s fall – and back to the gridiron (or ice rink, or soccer field) for young athletes throughout the region.
And while this is always an exciting time of year – it’s also prime time to talk about concussion.
Heightened media attention in recent years has led to greater awareness about this common form of mild traumatic brain injury (TBI) — as well as to greater concern among parents, coaches, and youth athletic leagues.
So much attention has been paid to the issue of youth head injuries that the Centers for Disease Control and Prevention (CDC) recently issued its first set of guidelines for treating mild TBI in children.
The good news is, sports and recreational activities are not the largest cause of brain injuries among children and adults. Simple slips and falls still reign supreme there — causing nearly 40 percent of concussions nationwide, according to the CDC.
While a fear of concussion should not deter you from letting your child play sports, children must play smart. Compared with student-athletes with no history of concussion, those who sustained a prior concussion are at greater risk of suffering another one – and it can take longer to recover from subsequent concussions.
There are no definitive guidelines for preventing concussions, but helmets, protective equipment, and fair-play rules remain the number one way to decrease the risk of serious brain injury and improve athlete safety.
Once an injury does occur – seeking the right type of treatment and rehabilitation is crucial. As neuropsychologists, we specialize in treating conditions affecting your brain. We’ve seen firsthand the difference the right experts can make in helping a client to recover and return to his or her life as quickly as possible.
And, again: Sports are not the only way to suffer a concussion. A simple slip and fall on an icy winter sidewalk can be just as risky – and to a much larger segment of the population – so these tips are worth remembering, no matter what you’re doing, where you’re going, or which activities your family is involved in.
Here are a few tips for parents facing their child’s first concussion – or concerned about what to do in the event of a future injury:
- Any player with a suspected concussion should be examined immediately by a licensed healthcare provider, who will decide when the child can resume playing. He or she can also help you decide what type of follow-up testing and evaluation may be needed.
- Neuropsychological testing is considered the cornerstone of sports concussion management – a tool that can help neuropsychologists identify cognitive symptoms related to concussion and make treatment recommendations. This information can also help inform your decisions about when your child should return to play, and any recommendations for their return to school and socialization.
- After a concussion, 24-48 hours of rest is recommended, followed by a gradual increase in activity.
- Anyone recovering from a concussion should avoid strenuous activity – and avoid activities that may exacerbate symptoms. Steer clear of video games, texting and television as much as possible. These activities can enhance the dizziness and nausea that often accompany a mild concussion, and can impede healing. As always, your child’s healthcare provider can guide you in deciding how much rest he or she needs.
Fortunately, many patients fully recover from mild concussions and suffer no long-term effects, especially after following the proper protocol and seeking the right kind of treatment. Most young athletes will recover from a concussion in less than four weeks; most adults, in less than two. If symptoms persist beyond this time frame, it may indicate a condition called “post-concussion syndrome,” and your child may benefit from additional treatment.
Whether on the field or walking down the street: Use extra caution and encourage your loved ones to do the same — and always consult your primary care physician to ensure proper diagnosis and treatment after an injury.


Dr. McGrath is the Senior Clinical Director for Bancroft NeuroRehab and co-director of postdoctoral training at Bancroft NeuroRehab. Dr. McGrath is board certified in clinical neuropsychology by the American Board of Professional Psychology. In her role at Bancroft NeuroRehab, she directs psychological and neuropsychological services at BNR’s 3 sites in Mt. Laurel, Plainsboro, and Toms River. She leads program development within the psychology department to advance neuropsychological assessment and psychological treatment for individuals in Bancroft NeuroRehab’s outpatient, residential, and day program services. Dr. McGrath also conducts neuropsychological evaluations of individuals with traumatic brain injury, stroke, dementia and other neurologic conditions.


Dr. Sarah West is an experienced Neuropsychologist who earned her master’s and doctoral degrees from Nova Southeastern University in Ft. Lauderdale, Fl. She completed her internship at the University of Alabama Birmingham and her postdoctoral fellowship at JFK-Johnson Rehabilitation Institute in Edison, NJ, where she conducted in-patient and outpatient neuropsychological assessments and therapy. Dr. West is a board-certified Neuropsychologist. She brings to Bancroft NeuroRehab a wide-reaching clinical background and specializes in Alzheimer’s disease, dementia, stroke and brain trauma. Dr. West’s research has been published in various trade journals, including The Encyclopedia of Neuropsychological Disorders and Brain Injury, among others. She has taught graduate courses in neuropsychology and is the co-director of the postdoctoral fellowship program at Bancroft NeuroRehab.